Yep you can’t get enough of”masks”to “SAVE MANKIND”!!! If you fools believe these masks save you then you certainly are the epitome of stupidity! And explaining the obvious would be a lesson in futility! But please continue your course because history will prove your ignorance in so much more detail than your numbers do now!
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
the great mask debate
- Thread starter diymirage
- Start date
-
RussellSullivan
Well-Known Member
Yep you can’t get enough of”masks”to “SAVE MANKIND”!!! If you fools believe these masks save you then you certainly are the epitome of stupidity! And explaining the obvious would be a lesson in futility! But please continue your course because history will prove your ignorance in so much more detail than your numbers do now!
The goal of this thread was to express our opinions about the masks, but do so while remaining civil. I wholeheartedly agree with your viewpoint, but there is a way to go about it and a way not to. Shouting from the rooftops about the intelligence/ignorance of others is no way of convincing them. If anything, it fosters even more hostility, and it doesn't do much good to the way people may perceive you, even if you are right. Take care now
Not only was my post opinion but mostly facts. I never tried to convince you or anyone else nor will I ever. Fear tactics work and in this instance-worked very well.The goal of this thread was to express our opinions about the masks, but do so while remaining civil. I wholeheartedly agree with your viewpoint, but there is a way to go about it and a way not to. Shouting from the rooftops about the intelligence/ignorance of others is no way of convincing them. If anything, it fosters even more hostility, and it doesn't do much good to the way people may perceive you, even if you are right. Take care now
The goal of this thread was to express our opinions about the masks, but do so while remaining civil. I wholeheartedly agree with your viewpoint, but there is a way to go about it and a way not to. Shouting from the rooftops about the intelligence/ignorance of others is no way of convincing them. If anything, it fosters even more hostility, and it doesn't do much good to the way people may perceive you, even if you are right. Take care now
like_A_pike
that's not factory
First I don't believe politicians and I don't subscribe to anything the media professes in editorial segments. I am a simple data analyst. I think, (that means this is an opinion of my own), that the mask is a pressure valve. Communities are desperate to keep businesses open and do as little damage to the economy if they can and certainly avoid lockdowns. the lynch pin to that is HOSPITAL CAPACITY. Since no-one can know how hard the funk will hit each of us, no-one can predict how many of us will need to visit the doctor. Ya'll know what its like when a simple cold goes around your community. I would bet that there is a lot of demographic probability going on in each of our communities and weighing that against how many people can get treated for whatever at any given time at the hospital. The mask isn't supposed to be the 100% way to not get the funk, and it certainly isn't supposed to save your life by itself. Its supposed to slow down how many of us get it at once so hospitals don't get overrun. I think that is how they supposedly save lives. Wear it, don't wear it, just keep an eye on local active case numbers and how your local hospital is coping with the load.... the communities that can't keep up at the ER are the ones talking lockdown.
I may be full of poop
I may be full of poop
norshorblufish
By the Big Water
Masks probably wont stop you from getting the virus by it self there are other factors also such as hygiene and social distancing.
To blast someone for wearing one is what’s the stupid part.
If you feel some what safer wearing one go ahead and wear one. My wife and I do when we go out to public places. we have family members with medical problems.
You will at least have a little protection.
Let’s say there are two people one with COVID and doesn’t have symptoms and the other that doesn’t have COVID nether wear masks. the possibility of the uninflected person is greater then if he wore one. And same if the other person was the only one to wear one.
If both wore a mask it would cut the chances even more because it would help cut the aerosol spray from breathing, talking, coughing, and sneezing.
To blast someone for wearing one is what’s the stupid part.
If you feel some what safer wearing one go ahead and wear one. My wife and I do when we go out to public places. we have family members with medical problems.
You will at least have a little protection.
Let’s say there are two people one with COVID and doesn’t have symptoms and the other that doesn’t have COVID nether wear masks. the possibility of the uninflected person is greater then if he wore one. And same if the other person was the only one to wear one.
If both wore a mask it would cut the chances even more because it would help cut the aerosol spray from breathing, talking, coughing, and sneezing.
Last edited:
SLOPAR72
Well-Known Member
Masks probably wont stop you from getting the virus by it self there are other factors also such as hygiene and social distancing.
To blast someone for wearing one is what’s the stupid part.
If you feel some what safer wearing one go ahead and wear one. My wife and I do we have family members with medical problems.
You will at least have a little protection.
Let’s say there are two people one with COVID and doesn’t have symptoms and the other that doesn’t have COVID nether wear masks. the possibility of the uninflected person is greater then if he wore one. And same if the other person was the only one to wear one.
Your choice. My choice. Don't force your agenda on me and vice versa. It's not that complicated so you are doing your thing. Just let me do mine.....
JW
If both wore a mask it would cut the chances even more because it would help cut the aerosol spray from breathing, talking, coughing, and sneezing.
First I don't believe politicians and I don't subscribe to anything the media professes in editorial segments. I am a simple data analyst. I think, (that means this is an opinion of my own), that the mask is a pressure valve. Communities are desperate to keep businesses open and do as little damage to the economy if they can and certainly avoid lockdowns. the lynch pin to that is HOSPITAL CAPACITY. Since no-one can know how hard the funk will hit each of us, no-one can predict how many of us will need to visit the doctor. Ya'll know what its like when a simple cold goes around your community. I would bet that there is a lot of demographic probability going on in each of our communities and weighing that against how many people can get treated for whatever at any given time at the hospital. The mask isn't supposed to be the 100% way to not get the funk, and it certainly isn't supposed to save your life by itself. Its supposed to slow down how many of us get it at once so hospitals don't get overrun. I think that is how they supposedly save lives. Wear it, don't wear it, just keep an eye on local active case numbers and how your local hospital is coping with the load.... the communities that can't keep up at the ER are the ones talking lockdown.
I may be full of poop
In VA. King Ralph (the governor) is actually a doctor and he has been ate up with it from day 1. Now we had it under control until the protest (which was perfectly ok) and since then the numbers went bonkers again. Pissed and sick of the whole thing. It's a political thing here. Wish my roots weren't planted like they are. I would be gone and the hell with these whacko's.....
JW
yellow rose
Overnight Sensation
Masks probably wont stop you from getting the virus by it self there are other factors also such as hygiene and social distancing.
To blast someone for wearing one is what’s the stupid part.
If you feel some what safer wearing one go ahead and wear one. My wife and I do we have family members with medical problems.
You will at least have a little protection.
Let’s say there are two people one with COVID and doesn’t have symptoms and the other that doesn’t have COVID nether wear masks. the possibility of the uninflected person is greater then if he wore one. And same if the other person was the only one to wear one.
If both wore a mask it would cut the chances even more because it would help cut the aerosol spray from breathing, talking, coughing, and sneezing.
I agree. If you think a mask works, wear one. If you think my not wearing a mask makes you unsafe, wear two masks. Wearing a mask for long periods is not good.
Back in Time
Well-Known Member
I wear mine in stores( mostly because it's mandatory here) and stay away from those that don't. That being said I don't shame anybody for not wearing one.
Yep! Wouldn’t it just be wonderful if anyone with any disease was confined to their bed and forced to wear a full face mask under hepafilters and banished from society until they had no symptoms of any kind! But let’s go to our food sources and water/sewer contamination’s. What is”acceptable” feces content?I wear mine in stores( mostly because it's mandatory here) and stay away from those that don't. That being said I don't shame anybody for not wearing one.
SLOPAR72
Well-Known Member
Yep! Wouldn’t it just be wonderful if anyone with any disease was confined to their bed and forced to wear a full face mask under hepafilters and banished from society until they had no symptoms of any kind! But let’s go to our food sources and water/sewer contamination’s. What is”acceptable” feces content?
You mean like the raw sewage they dump into our river in Richmond every Wednesday....... Yeah, that got swept right under the rug. Ain't no time for that.... Is that a floatie I see over there yonder......
JW
DodgeLad
Skipped the Light Fandango
mask or no mask, I love this guy
999yards
Well-Known Member
Already stated. Flatten the curve = lengthen the duration.
Everyone will get it.
"There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles.
Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective dose is smaller than one aerosol particle.
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
(From Words from the Publisher: "We pledge to publish all letters, guest commentaries, or studies refuting [Rancourt's] general premise that this mask-wearing culture and shaming could be more harmful than helpful. Please send your feedback to [email protected].") [UPDATE: August 12, 2020 Still No Evidence Justifying Mandatory Masks]
Review of the Medical Literature
Here are key anchor points to the extensive scientific literature that establishes that wearing surgical masks and respirators (e.g., “N95”) does not reduce the risk of contracting a verified illness:
Jacobs, J. L. et al. (2009) “Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial,” American Journal of Infection Control, Volume 37, Issue 5, 417 – 419. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial - PubMed
N95-masked health-care workers (HCW) were significantly more likely to experience headaches. Face mask use in HCW was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
Cowling, B. et al. (2010) “Face masks to prevent transmission of influenza virus: A systematic review,” Epidemiology and Infection, 138(4), 449-456. https://www.cambridge.org/core/journals/epidemiology-and-infection/article/face-masks-to-prevent-transmission-of-influenza-virus-a-systematic- review/64D368496EBDE0AFCC6639CCC9D8BC05
None of the studies reviewed showed a benefit from wearing a mask, in either HCW or community members in households (H). See summary Tables 1 and 2 therein.
bin-Reza et al. (2012) “The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence,” Influenza and Other Respiratory Viruses 6(4), 257–267. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1750-2659.2011.00307.x
“There were 17 eligible studies. … None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”
Smith, J.D. et al. (2016) “Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis,” CMAJ Mar 2016 Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis
“We identified six clinical studies … . In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
Offeddu, V. et al. (2017) “Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis,” Clinical Infectious Diseases, Volume 65, Issue 11, 1 December 2017, Pages 1934–1942, Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis
“Self-reported assessment of clinical outcomes was prone to bias. Evidence of a protective effect of masks or respirators against verified respiratory infection (VRI) was not statistically significant”; as per Fig. 2c therein:

Radonovich, L.J. et al. (2019) “N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial,” JAMA. 2019; 322(9): 824–833. N95 Respirators vs Medical Masks for Preventing Laboratory-Confirmed Influenza in Health Care Personnel
“Among 2862 randomized participants, 2371 completed the study and accounted for 5180 HCW-seasons. ... Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.”
Long, Y. et al. (2020) “Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis,” J Evid Based Med. 2020; 1- 9. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381
“A total of six RCTs involving 9,171 participants were included. There were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection, and influenza-like illness using N95 respirators and surgical masks. Meta-analysis indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78). The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza.”
Conclusion Regarding That Masks Do Not Work
No RCT study with verified outcome shows a benefit for HCW or community members in households to wearing a mask or respirator. There is no such study. There are no exceptions.
Likewise, no study exists that shows a benefit from a broad policy to wear masks in public (more on this below).
Furthermore, if there were any benefit to wearing a mask, because of the blocking power against droplets and aerosol particles, then there should be more benefit from wearing a respirator (N95) compared to a surgical mask, yet several large meta-analyses, and all the RCT, prove that there is no such relative benefit.
Masks and respirators do not work.
Precautionary Principle Turned on Its Head with Masks
In light of the medical research, therefore, it is difficult to understand why public-health authorities are not consistently adamant about this established scientific result, since the distributed psychological, economic, and environmental harm from a broad recommendation to wear masks is significant, not to mention the unknown potential harm from concentration and distribution of pathogens on and from used masks. In this case, public authorities would be turning the precautionary principle on its head (see below).
Physics and Biology of Viral Respiratory Disease and of Why Masks Do Not Work
In order to understand why masks cannot possibly work, we must review established knowledge about viral respiratory diseases, the mechanism of seasonal variation of excess deaths from pneumonia and influenza, the aerosol mechanism of infectious disease transmission, the physics and chemistry of aerosols, and the mechanism of the so-called minimum-infective-dose.
In addition to pandemics that can occur anytime, in the temperate latitudes there is an extra burden of respiratory-disease mortality that is seasonal, and that is caused by viruses. For example, see the review of influenza by Paules and Subbarao (2017). This has been known for a long time, and the seasonal pattern is exceedingly regular. (Publisher's note: All links to source references to studies here forward are found at the end of this article.)
For example, see Figure 1 of Viboud (2010), which has “Weekly time series of the ratio of deaths from pneumonia and influenza to all deaths, based on the 122 cities surveillance in the US (blue line). The red line represents the expected baseline ratio in the absence of influenza activity,” here:

The seasonality of the phenomenon was largely not understood until a decade ago. Until recently, it was debated whether the pattern arose primarily because of seasonal change in virulence of the pathogens, or because of seasonal change in susceptibility of the host (such as from dry air causing tissue irritation, or diminished daylight causing vitamin deficiency or hormonal stress). For example, see Dowell (2001).
In a landmark study, Shaman et al. (2010) showed that the seasonal pattern of extra respiratory-disease mortality can be explained quantitatively on the sole basis of absolute humidity, and its direct controlling impact on transmission of airborne pathogens.
Lowen et al. (2007) demonstrated the phenomenon of humidity-dependent airborne-virus virulence in actual disease transmission between guinea pigs, and discussed potential underlying mechanisms for the measured controlling effect of humidity.
The underlying mechanism is that the pathogen-laden aerosol particles or droplets are neutralized within a half-life that monotonically and significantly decreases with increasing ambient humidity. This is based on the seminal work of Harper (1961). Harper experimentally showed that viral-pathogen-carrying droplets were inactivated within shorter and shorter times, as ambient humidity was increased.
Harper argued that the viruses themselves were made inoperative by the humidity (“viable decay”), however, he admitted that the effect could be from humidity-enhanced physical removal or sedimentation of the droplets (“physical loss”): “Aerosol viabilities reported in this paper are based on the ratio of virus titre to radioactive count in suspension and cloud samples, and can be criticized on the ground that test and tracer materials were not physically identical.”
The latter (“physical loss”) seems more plausible to me, since humidity would have a universal physical effect of causing particle/droplet growth and sedimentation, and all tested viral pathogens have essentially the same humidity-driven “decay.” Furthermore, it is difficult to understand how a virion (of all virus types) in a droplet would be molecularly or structurally attacked or damaged by an increase in ambient humidity. A “virion” is the complete, infective form of a virus outside a host cell, with a core of RNA or DNA and a capsid. The actual mechanism of such humidity-driven intra-droplet “viable decay” of a virion has not been explained or studied.
In any case, the explanation and model of Shaman et al. (2010) is not dependent on the particular mechanism of the humidity-driven decay of virions in aerosol/droplets. Shaman’s quantitatively demonstrated model of seasonal regional viral epidemiology is valid for either mechanism (or combination of mechanisms), whether “viable decay” or “physical loss.”
The breakthrough achieved by Shaman et al. is not merely some academic point. Rather, it has profound health-policy implications, which have been entirely ignored or overlooked in the current coronavirus pandemic.
In particular, Shaman’s work necessarily implies that, rather than being a fixed number (dependent solely on the spatial-temporal structure of social interactions in a completely susceptible population, and on the viral strain), the epidemic’s basic reproduction number (R0) is highly or predominantly dependent on ambient absolute humidity.
For a definition of R0, see HealthKnowlege-UK (2020): R0 is “the average number of secondary infections produced by a typical case of an infection in a population where everyone is susceptible.” The average R0 for influenza is said to be 1.28 (1.19–1.37); see the comprehensive review by Biggerstaff et al. (2014).
In fact, Shaman et al. showed that R0 must be understood to seasonally vary between humid-summer values of just larger than “1” and dry-winter values typically as large as “4” (for example, see their Table 2). In other words, the seasonal infectious viral respiratory diseases that plague temperate latitudes every year go from being intrinsically mildly contagious to virulently contagious, due simply to the bio-physical mode of transmission controlled by atmospheric humidity, irrespective of any other consideration.
Therefore, all the epidemiological mathematical modeling of the benefits of mediating policies (such as social distancing), which assumes humidity-independent R0 values, has a large likelihood of being of little value, on this basis alone. For studies about modeling and regarding mediation effects on the effective reproduction number, see Coburn (2009) and Tracht (2010).
To put it simply, the “second wave” of an epidemic is not a consequence of human sin regarding mask wearing and hand shaking. Rather, the “second wave” is an inescapable consequence of an air-dryness-driven many-fold increase in disease contagiousness, in a population that has not yet attained immunity.
If my view of the mechanism is correct (i.e., “physical loss”), then Shaman’s work further necessarily implies that the dryness-driven high transmissibility (large R0) arises from small aerosol particles fluidly suspended in the air; as opposed to large droplets that are quickly gravitationally removed from the air.
Such small aerosol particles fluidly suspended in air, of biological origin, are of every variety and are everywhere, including down to virion-sizes (Despres, 2012). It is not entirely unlikely that viruses can thereby be physically transported over inter-continental distances (e.g., Hammond, 1989).
More to the point, indoor airborne virus concentrations have been shown to exist (in day-care facilities, health centers, and on-board airplanes) primarily as aerosol particles of diameters smaller than 2.5 μm, such as in the work of Yang et al. (2011):
“Half of the 16 samples were positive, and their total virus −3 concentrations ranged from 5800 to 37 000 genome copies m . On average, 64 per cent of the viral genome copies were associated with fine particles smaller than 2.5 μm, which can remain suspended for hours. Modeling of virus concentrations indoors suggested a source strength of 1.6 ± 1.2 × 105 genome copies m−3 air h−1 and a deposition flux onto surfaces of 13 ± 7 genome copies m−2 h−1 by Brownian motion. Over one hour, the inhalation dose was estimated to be 30 ± 18 median tissue culture infectious dose (TCID50), adequate to induce infection. These results provide quantitative support for the idea that the aerosol route could be an important mode of influenza transmission.”
Such small particles (< 2.5 μm) are part of air fluidity, are not subject to gravitational sedimentation, and would not be stopped by long-range inertial impact. This means that the slightest (even momentary) facial misfit of a mask or respirator renders the design filtration norm of the mask or respirator entirely irrelevant. In any case, the filtration material itself of N95 (average pore size ~0.3−0.5 μm) does not block virion penetration, not to mention surgical masks. For example, see Balazy et al. (2006).
Mask stoppage efficiency and host inhalation are only half of the equation, however, because the minimal infective dose (MID) must also be considered. For example, if a large number of pathogen-laden particles must be delivered to the lung within a certain time for the illness to take hold, then partial blocking by any mask or cloth can be enough to make a significant difference.
On the other hand, if the MID is amply surpassed by the virions carried in a single aerosol particle able to evade mask-capture, then the mask is of no practical utility, which is the case.
Yezli and Otter (2011), in their review of the MID, point out relevant features:
Therefore, the studies that show partial stopping power of masks, or that show that masks can capture many large droplets produced by a sneezing or coughing mask-wearer, in light of the above-described features of the problem, are irrelevant. For example, such studies as these: Leung (2020), Davies (2013), Lai (2012), and Sande (2008).
Why There Can Never Be an Empirical Test of a Nation-Wide Mask-Wearing Policy
As mentioned above, no study exists that shows a benefit from a broad policy to wear masks in public. There is good reason for this. It would be impossible to obtain unambiguous and bias-free results [because]:
Many potential harms may arise from broad public policies to wear masks, and the following unanswered questions arise:
By making mask-wearing recommendations and policies for the general public, or by expressly condoning the practice, governments have both ignored the scientific evidence and done the opposite of following the precautionary principle.
In an absence of knowledge, governments should not make policies that have a hypothetical potential to cause harm. The government has an onus barrier before it instigates a broad social-engineering intervention, or allows corporations to exploit fear-based sentiments.
Furthermore, individuals should know that there is no known benefit arising from wearing a mask in a viral respiratory illness epidemic, and that scientific studies have shown that any benefit must be residually small, compared to other and determinative factors.
Otherwise, what is the point of publicly funded science?
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
Denis G. Rancourt is a researcher at the Ontario Civil Liberties Association (OCLA.ca) and is formerly a tenured professor at the University of Ottawa, Canada. This paper was originally published at Rancourt's account on ResearchGate.net. As of June 5, 2020, this paper was removed from his profile by its administrators at Researchgate.net/profile/D_Rancourt. At Rancourt's blog ActivistTeacher.blogspot.com, he recounts the notification and responses he received from ResearchGate.net and states, “This is censorship of my scientific work like I have never experienced before.”
The original April 2020 white paper in .pdf format is available here, complete with charts that have not been reprinted in the Reader print or web versions.
Everyone will get it.
"There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles.
Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective dose is smaller than one aerosol particle.
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
(From Words from the Publisher: "We pledge to publish all letters, guest commentaries, or studies refuting [Rancourt's] general premise that this mask-wearing culture and shaming could be more harmful than helpful. Please send your feedback to [email protected].") [UPDATE: August 12, 2020 Still No Evidence Justifying Mandatory Masks]
Review of the Medical Literature
Here are key anchor points to the extensive scientific literature that establishes that wearing surgical masks and respirators (e.g., “N95”) does not reduce the risk of contracting a verified illness:
Jacobs, J. L. et al. (2009) “Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial,” American Journal of Infection Control, Volume 37, Issue 5, 417 – 419. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial - PubMed
N95-masked health-care workers (HCW) were significantly more likely to experience headaches. Face mask use in HCW was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
Cowling, B. et al. (2010) “Face masks to prevent transmission of influenza virus: A systematic review,” Epidemiology and Infection, 138(4), 449-456. https://www.cambridge.org/core/journals/epidemiology-and-infection/article/face-masks-to-prevent-transmission-of-influenza-virus-a-systematic- review/64D368496EBDE0AFCC6639CCC9D8BC05
None of the studies reviewed showed a benefit from wearing a mask, in either HCW or community members in households (H). See summary Tables 1 and 2 therein.
bin-Reza et al. (2012) “The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence,” Influenza and Other Respiratory Viruses 6(4), 257–267. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1750-2659.2011.00307.x
“There were 17 eligible studies. … None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”
Smith, J.D. et al. (2016) “Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis,” CMAJ Mar 2016 Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis
“We identified six clinical studies … . In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
Offeddu, V. et al. (2017) “Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis,” Clinical Infectious Diseases, Volume 65, Issue 11, 1 December 2017, Pages 1934–1942, Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis
“Self-reported assessment of clinical outcomes was prone to bias. Evidence of a protective effect of masks or respirators against verified respiratory infection (VRI) was not statistically significant”; as per Fig. 2c therein:
Radonovich, L.J. et al. (2019) “N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial,” JAMA. 2019; 322(9): 824–833. N95 Respirators vs Medical Masks for Preventing Laboratory-Confirmed Influenza in Health Care Personnel
“Among 2862 randomized participants, 2371 completed the study and accounted for 5180 HCW-seasons. ... Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.”
Long, Y. et al. (2020) “Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis,” J Evid Based Med. 2020; 1- 9. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381
“A total of six RCTs involving 9,171 participants were included. There were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection, and influenza-like illness using N95 respirators and surgical masks. Meta-analysis indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78). The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza.”
Conclusion Regarding That Masks Do Not Work
No RCT study with verified outcome shows a benefit for HCW or community members in households to wearing a mask or respirator. There is no such study. There are no exceptions.
Likewise, no study exists that shows a benefit from a broad policy to wear masks in public (more on this below).
Furthermore, if there were any benefit to wearing a mask, because of the blocking power against droplets and aerosol particles, then there should be more benefit from wearing a respirator (N95) compared to a surgical mask, yet several large meta-analyses, and all the RCT, prove that there is no such relative benefit.
Masks and respirators do not work.
Precautionary Principle Turned on Its Head with Masks
In light of the medical research, therefore, it is difficult to understand why public-health authorities are not consistently adamant about this established scientific result, since the distributed psychological, economic, and environmental harm from a broad recommendation to wear masks is significant, not to mention the unknown potential harm from concentration and distribution of pathogens on and from used masks. In this case, public authorities would be turning the precautionary principle on its head (see below).
Physics and Biology of Viral Respiratory Disease and of Why Masks Do Not Work
In order to understand why masks cannot possibly work, we must review established knowledge about viral respiratory diseases, the mechanism of seasonal variation of excess deaths from pneumonia and influenza, the aerosol mechanism of infectious disease transmission, the physics and chemistry of aerosols, and the mechanism of the so-called minimum-infective-dose.
In addition to pandemics that can occur anytime, in the temperate latitudes there is an extra burden of respiratory-disease mortality that is seasonal, and that is caused by viruses. For example, see the review of influenza by Paules and Subbarao (2017). This has been known for a long time, and the seasonal pattern is exceedingly regular. (Publisher's note: All links to source references to studies here forward are found at the end of this article.)
For example, see Figure 1 of Viboud (2010), which has “Weekly time series of the ratio of deaths from pneumonia and influenza to all deaths, based on the 122 cities surveillance in the US (blue line). The red line represents the expected baseline ratio in the absence of influenza activity,” here:
The seasonality of the phenomenon was largely not understood until a decade ago. Until recently, it was debated whether the pattern arose primarily because of seasonal change in virulence of the pathogens, or because of seasonal change in susceptibility of the host (such as from dry air causing tissue irritation, or diminished daylight causing vitamin deficiency or hormonal stress). For example, see Dowell (2001).
In a landmark study, Shaman et al. (2010) showed that the seasonal pattern of extra respiratory-disease mortality can be explained quantitatively on the sole basis of absolute humidity, and its direct controlling impact on transmission of airborne pathogens.
Lowen et al. (2007) demonstrated the phenomenon of humidity-dependent airborne-virus virulence in actual disease transmission between guinea pigs, and discussed potential underlying mechanisms for the measured controlling effect of humidity.
The underlying mechanism is that the pathogen-laden aerosol particles or droplets are neutralized within a half-life that monotonically and significantly decreases with increasing ambient humidity. This is based on the seminal work of Harper (1961). Harper experimentally showed that viral-pathogen-carrying droplets were inactivated within shorter and shorter times, as ambient humidity was increased.
Harper argued that the viruses themselves were made inoperative by the humidity (“viable decay”), however, he admitted that the effect could be from humidity-enhanced physical removal or sedimentation of the droplets (“physical loss”): “Aerosol viabilities reported in this paper are based on the ratio of virus titre to radioactive count in suspension and cloud samples, and can be criticized on the ground that test and tracer materials were not physically identical.”
The latter (“physical loss”) seems more plausible to me, since humidity would have a universal physical effect of causing particle/droplet growth and sedimentation, and all tested viral pathogens have essentially the same humidity-driven “decay.” Furthermore, it is difficult to understand how a virion (of all virus types) in a droplet would be molecularly or structurally attacked or damaged by an increase in ambient humidity. A “virion” is the complete, infective form of a virus outside a host cell, with a core of RNA or DNA and a capsid. The actual mechanism of such humidity-driven intra-droplet “viable decay” of a virion has not been explained or studied.
In any case, the explanation and model of Shaman et al. (2010) is not dependent on the particular mechanism of the humidity-driven decay of virions in aerosol/droplets. Shaman’s quantitatively demonstrated model of seasonal regional viral epidemiology is valid for either mechanism (or combination of mechanisms), whether “viable decay” or “physical loss.”
The breakthrough achieved by Shaman et al. is not merely some academic point. Rather, it has profound health-policy implications, which have been entirely ignored or overlooked in the current coronavirus pandemic.
In particular, Shaman’s work necessarily implies that, rather than being a fixed number (dependent solely on the spatial-temporal structure of social interactions in a completely susceptible population, and on the viral strain), the epidemic’s basic reproduction number (R0) is highly or predominantly dependent on ambient absolute humidity.
For a definition of R0, see HealthKnowlege-UK (2020): R0 is “the average number of secondary infections produced by a typical case of an infection in a population where everyone is susceptible.” The average R0 for influenza is said to be 1.28 (1.19–1.37); see the comprehensive review by Biggerstaff et al. (2014).
In fact, Shaman et al. showed that R0 must be understood to seasonally vary between humid-summer values of just larger than “1” and dry-winter values typically as large as “4” (for example, see their Table 2). In other words, the seasonal infectious viral respiratory diseases that plague temperate latitudes every year go from being intrinsically mildly contagious to virulently contagious, due simply to the bio-physical mode of transmission controlled by atmospheric humidity, irrespective of any other consideration.
Therefore, all the epidemiological mathematical modeling of the benefits of mediating policies (such as social distancing), which assumes humidity-independent R0 values, has a large likelihood of being of little value, on this basis alone. For studies about modeling and regarding mediation effects on the effective reproduction number, see Coburn (2009) and Tracht (2010).
To put it simply, the “second wave” of an epidemic is not a consequence of human sin regarding mask wearing and hand shaking. Rather, the “second wave” is an inescapable consequence of an air-dryness-driven many-fold increase in disease contagiousness, in a population that has not yet attained immunity.
If my view of the mechanism is correct (i.e., “physical loss”), then Shaman’s work further necessarily implies that the dryness-driven high transmissibility (large R0) arises from small aerosol particles fluidly suspended in the air; as opposed to large droplets that are quickly gravitationally removed from the air.
Such small aerosol particles fluidly suspended in air, of biological origin, are of every variety and are everywhere, including down to virion-sizes (Despres, 2012). It is not entirely unlikely that viruses can thereby be physically transported over inter-continental distances (e.g., Hammond, 1989).
More to the point, indoor airborne virus concentrations have been shown to exist (in day-care facilities, health centers, and on-board airplanes) primarily as aerosol particles of diameters smaller than 2.5 μm, such as in the work of Yang et al. (2011):
“Half of the 16 samples were positive, and their total virus −3 concentrations ranged from 5800 to 37 000 genome copies m . On average, 64 per cent of the viral genome copies were associated with fine particles smaller than 2.5 μm, which can remain suspended for hours. Modeling of virus concentrations indoors suggested a source strength of 1.6 ± 1.2 × 105 genome copies m−3 air h−1 and a deposition flux onto surfaces of 13 ± 7 genome copies m−2 h−1 by Brownian motion. Over one hour, the inhalation dose was estimated to be 30 ± 18 median tissue culture infectious dose (TCID50), adequate to induce infection. These results provide quantitative support for the idea that the aerosol route could be an important mode of influenza transmission.”
Such small particles (< 2.5 μm) are part of air fluidity, are not subject to gravitational sedimentation, and would not be stopped by long-range inertial impact. This means that the slightest (even momentary) facial misfit of a mask or respirator renders the design filtration norm of the mask or respirator entirely irrelevant. In any case, the filtration material itself of N95 (average pore size ~0.3−0.5 μm) does not block virion penetration, not to mention surgical masks. For example, see Balazy et al. (2006).
Mask stoppage efficiency and host inhalation are only half of the equation, however, because the minimal infective dose (MID) must also be considered. For example, if a large number of pathogen-laden particles must be delivered to the lung within a certain time for the illness to take hold, then partial blocking by any mask or cloth can be enough to make a significant difference.
On the other hand, if the MID is amply surpassed by the virions carried in a single aerosol particle able to evade mask-capture, then the mask is of no practical utility, which is the case.
Yezli and Otter (2011), in their review of the MID, point out relevant features:
- Most respiratory viruses are as infective in humans as in tissue culture having optimal laboratory susceptibility
- It is believed that a single virion can be enough to induce illness in the host
- The 50-percent probability MID (“TCID50”) has variably been found to be in the range 100−1000 virions
- There are typically 10 to 3rd power − 10 to 7th power virions per aerolized influenza droplet with diameter 1 μm − 10 μm
- The 50-percent probability MID easily fits into a single (one) aerolized droplet
- For further background:
- A classic description of dose-response assessment is provided by Haas (1993).
- Zwart et al. (2009) provided the first laboratory proof, in a virus-insect system, that the action of a single virion can be sufficient to cause disease.
- Baccam et al. (2006) calculated from empirical data that, with influenza A in humans,“we estimate that after a delay of ~6 h, infected cells begin producing influenza virus and continue to do so for ~5 h. The average lifetime of infected cells is ~11 h, and the half-life of free infectious virus is ~3 h. We calculated the [in-body] basic reproductive number, R0, which indicated that a single infected cell could produce ~22 new productive infections.”
- Brooke et al. (2013) showed that, contrary to prior modeling assumptions, although not all influenza-A-infected cells in the human body produce infectious progeny (virions), nonetheless, 90 percent of infected cell are significantly impacted, rather than simply surviving unharmed.
Therefore, the studies that show partial stopping power of masks, or that show that masks can capture many large droplets produced by a sneezing or coughing mask-wearer, in light of the above-described features of the problem, are irrelevant. For example, such studies as these: Leung (2020), Davies (2013), Lai (2012), and Sande (2008).
Why There Can Never Be an Empirical Test of a Nation-Wide Mask-Wearing Policy
As mentioned above, no study exists that shows a benefit from a broad policy to wear masks in public. There is good reason for this. It would be impossible to obtain unambiguous and bias-free results [because]:
- Any benefit from mask-wearing would have to be a small effect, since undetected in controlled experiments, which would be swamped by the larger effects, notably the large effect from changing atmospheric humidity.
- Mask compliance and mask adjustment habits would be unknown.
- Mask-wearing is associated (correlated) with several other health behaviors; see Wada (2012).
- The results would not be transferable, because of differing cultural habits.
- Compliance is achieved by fear, and individuals can habituate to fear-based propaganda, and can have disparate basic responses.
- Monitoring and compliance measurement are near-impossible, and subject to large errors.
- Self-reporting (such as in surveys) is notoriously biased, because individuals have the self-interested belief that their efforts are useful.
- Progression of the epidemic is not verified with reliable tests on large population samples, and generally relies on non-representative hospital visits or admissions.
- Several different pathogens (viruses and strains of viruses) causing respiratory illness generally act together, in the same population and/or in individuals, and are not resolved, while having different epidemiological characteristics.
Many potential harms may arise from broad public policies to wear masks, and the following unanswered questions arise:
- Do used and loaded masks become sources of enhanced transmission, for the wearer and others?
- Do masks become collectors and retainers of pathogens that the mask wearer would otherwise avoid when breathing without a mask?
- Are large droplets captured by a mask atomized or aerolized into breathable components? Can virions escape an evaporating droplet stuck to a mask fiber?
- What are the dangers of bacterial growth on a used and loaded mask?
- How do pathogen-laden droplets interact with environmental dust and aerosols captured on the mask?
- What are long-term health effects on HCW, such as headaches, arising from impeded breathing?
- Are there negative social consequences to a masked society?
- Are there negative psychological consequences to wearing a mask, as a fear-based behavioral modification?
- What are the environmental consequences of mask manufacturing and disposal?
- Do the masks shed fibers or substances that are harmful when inhaled?
By making mask-wearing recommendations and policies for the general public, or by expressly condoning the practice, governments have both ignored the scientific evidence and done the opposite of following the precautionary principle.
In an absence of knowledge, governments should not make policies that have a hypothetical potential to cause harm. The government has an onus barrier before it instigates a broad social-engineering intervention, or allows corporations to exploit fear-based sentiments.
Furthermore, individuals should know that there is no known benefit arising from wearing a mask in a viral respiratory illness epidemic, and that scientific studies have shown that any benefit must be residually small, compared to other and determinative factors.
Otherwise, what is the point of publicly funded science?
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
Denis G. Rancourt is a researcher at the Ontario Civil Liberties Association (OCLA.ca) and is formerly a tenured professor at the University of Ottawa, Canada. This paper was originally published at Rancourt's account on ResearchGate.net. As of June 5, 2020, this paper was removed from his profile by its administrators at Researchgate.net/profile/D_Rancourt. At Rancourt's blog ActivistTeacher.blogspot.com, he recounts the notification and responses he received from ResearchGate.net and states, “This is censorship of my scientific work like I have never experienced before.”
The original April 2020 white paper in .pdf format is available here, complete with charts that have not been reprinted in the Reader print or web versions.
Last edited:
yellow rose
Overnight Sensation
Already stated. Flatten the curve = lengthen the duration.
Everyone will get it.
"There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles.
Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective dose is smaller than one aerosol particle.
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
(From Words from the Publisher: "We pledge to publish all letters, guest commentaries, or studies refuting [Rancourt's] general premise that this mask-wearing culture and shaming could be more harmful than helpful. Please send your feedback to [email protected].") [UPDATE: August 12, 2020 Still No Evidence Justifying Mandatory Masks]
Review of the Medical Literature
Here are key anchor points to the extensive scientific literature that establishes that wearing surgical masks and respirators (e.g., “N95”) does not reduce the risk of contracting a verified illness:
Jacobs, J. L. et al. (2009) “Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial,” American Journal of Infection Control, Volume 37, Issue 5, 417 – 419. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial - PubMed
N95-masked health-care workers (HCW) were significantly more likely to experience headaches. Face mask use in HCW was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
Cowling, B. et al. (2010) “Face masks to prevent transmission of influenza virus: A systematic review,” Epidemiology and Infection, 138(4), 449-456. https://www.cambridge.org/core/journals/epidemiology-and-infection/article/face-masks-to-prevent-transmission-of-influenza-virus-a-systematic- review/64D368496EBDE0AFCC6639CCC9D8BC05
None of the studies reviewed showed a benefit from wearing a mask, in either HCW or community members in households (H). See summary Tables 1 and 2 therein.
bin-Reza et al. (2012) “The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence,” Influenza and Other Respiratory Viruses 6(4), 257–267. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1750-2659.2011.00307.x
“There were 17 eligible studies. … None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”
Smith, J.D. et al. (2016) “Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis,” CMAJ Mar 2016 Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis
“We identified six clinical studies … . In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
Offeddu, V. et al. (2017) “Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis,” Clinical Infectious Diseases, Volume 65, Issue 11, 1 December 2017, Pages 1934–1942, Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis
“Self-reported assessment of clinical outcomes was prone to bias. Evidence of a protective effect of masks or respirators against verified respiratory infection (VRI) was not statistically significant”; as per Fig. 2c therein:

Radonovich, L.J. et al. (2019) “N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial,” JAMA. 2019; 322(9): 824–833. N95 Respirators vs Medical Masks for Preventing Laboratory-Confirmed Influenza in Health Care Personnel
“Among 2862 randomized participants, 2371 completed the study and accounted for 5180 HCW-seasons. ... Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.”
Long, Y. et al. (2020) “Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis,” J Evid Based Med. 2020; 1- 9. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381
“A total of six RCTs involving 9,171 participants were included. There were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection, and influenza-like illness using N95 respirators and surgical masks. Meta-analysis indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78). The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza.”
Conclusion Regarding That Masks Do Not Work
No RCT study with verified outcome shows a benefit for HCW or community members in households to wearing a mask or respirator. There is no such study. There are no exceptions.
Likewise, no study exists that shows a benefit from a broad policy to wear masks in public (more on this below).
Furthermore, if there were any benefit to wearing a mask, because of the blocking power against droplets and aerosol particles, then there should be more benefit from wearing a respirator (N95) compared to a surgical mask, yet several large meta-analyses, and all the RCT, prove that there is no such relative benefit.
Masks and respirators do not work.
Precautionary Principle Turned on Its Head with Masks
In light of the medical research, therefore, it is difficult to understand why public-health authorities are not consistently adamant about this established scientific result, since the distributed psychological, economic, and environmental harm from a broad recommendation to wear masks is significant, not to mention the unknown potential harm from concentration and distribution of pathogens on and from used masks. In this case, public authorities would be turning the precautionary principle on its head (see below).
Physics and Biology of Viral Respiratory Disease and of Why Masks Do Not Work
In order to understand why masks cannot possibly work, we must review established knowledge about viral respiratory diseases, the mechanism of seasonal variation of excess deaths from pneumonia and influenza, the aerosol mechanism of infectious disease transmission, the physics and chemistry of aerosols, and the mechanism of the so-called minimum-infective-dose.
In addition to pandemics that can occur anytime, in the temperate latitudes there is an extra burden of respiratory-disease mortality that is seasonal, and that is caused by viruses. For example, see the review of influenza by Paules and Subbarao (2017). This has been known for a long time, and the seasonal pattern is exceedingly regular. (Publisher's note: All links to source references to studies here forward are found at the end of this article.)
For example, see Figure 1 of Viboud (2010), which has “Weekly time series of the ratio of deaths from pneumonia and influenza to all deaths, based on the 122 cities surveillance in the US (blue line). The red line represents the expected baseline ratio in the absence of influenza activity,” here:

The seasonality of the phenomenon was largely not understood until a decade ago. Until recently, it was debated whether the pattern arose primarily because of seasonal change in virulence of the pathogens, or because of seasonal change in susceptibility of the host (such as from dry air causing tissue irritation, or diminished daylight causing vitamin deficiency or hormonal stress). For example, see Dowell (2001).
In a landmark study, Shaman et al. (2010) showed that the seasonal pattern of extra respiratory-disease mortality can be explained quantitatively on the sole basis of absolute humidity, and its direct controlling impact on transmission of airborne pathogens.
Lowen et al. (2007) demonstrated the phenomenon of humidity-dependent airborne-virus virulence in actual disease transmission between guinea pigs, and discussed potential underlying mechanisms for the measured controlling effect of humidity.
The underlying mechanism is that the pathogen-laden aerosol particles or droplets are neutralized within a half-life that monotonically and significantly decreases with increasing ambient humidity. This is based on the seminal work of Harper (1961). Harper experimentally showed that viral-pathogen-carrying droplets were inactivated within shorter and shorter times, as ambient humidity was increased.
Harper argued that the viruses themselves were made inoperative by the humidity (“viable decay”), however, he admitted that the effect could be from humidity-enhanced physical removal or sedimentation of the droplets (“physical loss”): “Aerosol viabilities reported in this paper are based on the ratio of virus titre to radioactive count in suspension and cloud samples, and can be criticized on the ground that test and tracer materials were not physically identical.”
The latter (“physical loss”) seems more plausible to me, since humidity would have a universal physical effect of causing particle/droplet growth and sedimentation, and all tested viral pathogens have essentially the same humidity-driven “decay.” Furthermore, it is difficult to understand how a virion (of all virus types) in a droplet would be molecularly or structurally attacked or damaged by an increase in ambient humidity. A “virion” is the complete, infective form of a virus outside a host cell, with a core of RNA or DNA and a capsid. The actual mechanism of such humidity-driven intra-droplet “viable decay” of a virion has not been explained or studied.
In any case, the explanation and model of Shaman et al. (2010) is not dependent on the particular mechanism of the humidity-driven decay of virions in aerosol/droplets. Shaman’s quantitatively demonstrated model of seasonal regional viral epidemiology is valid for either mechanism (or combination of mechanisms), whether “viable decay” or “physical loss.”
The breakthrough achieved by Shaman et al. is not merely some academic point. Rather, it has profound health-policy implications, which have been entirely ignored or overlooked in the current coronavirus pandemic.
In particular, Shaman’s work necessarily implies that, rather than being a fixed number (dependent solely on the spatial-temporal structure of social interactions in a completely susceptible population, and on the viral strain), the epidemic’s basic reproduction number (R0) is highly or predominantly dependent on ambient absolute humidity.
For a definition of R0, see HealthKnowlege-UK (2020): R0 is “the average number of secondary infections produced by a typical case of an infection in a population where everyone is susceptible.” The average R0 for influenza is said to be 1.28 (1.19–1.37); see the comprehensive review by Biggerstaff et al. (2014).
In fact, Shaman et al. showed that R0 must be understood to seasonally vary between humid-summer values of just larger than “1” and dry-winter values typically as large as “4” (for example, see their Table 2). In other words, the seasonal infectious viral respiratory diseases that plague temperate latitudes every year go from being intrinsically mildly contagious to virulently contagious, due simply to the bio-physical mode of transmission controlled by atmospheric humidity, irrespective of any other consideration.
Therefore, all the epidemiological mathematical modeling of the benefits of mediating policies (such as social distancing), which assumes humidity-independent R0 values, has a large likelihood of being of little value, on this basis alone. For studies about modeling and regarding mediation effects on the effective reproduction number, see Coburn (2009) and Tracht (2010).
To put it simply, the “second wave” of an epidemic is not a consequence of human sin regarding mask wearing and hand shaking. Rather, the “second wave” is an inescapable consequence of an air-dryness-driven many-fold increase in disease contagiousness, in a population that has not yet attained immunity.
If my view of the mechanism is correct (i.e., “physical loss”), then Shaman’s work further necessarily implies that the dryness-driven high transmissibility (large R0) arises from small aerosol particles fluidly suspended in the air; as opposed to large droplets that are quickly gravitationally removed from the air.
Such small aerosol particles fluidly suspended in air, of biological origin, are of every variety and are everywhere, including down to virion-sizes (Despres, 2012). It is not entirely unlikely that viruses can thereby be physically transported over inter-continental distances (e.g., Hammond, 1989).
More to the point, indoor airborne virus concentrations have been shown to exist (in day-care facilities, health centers, and on-board airplanes) primarily as aerosol particles of diameters smaller than 2.5 μm, such as in the work of Yang et al. (2011):
“Half of the 16 samples were positive, and their total virus −3 concentrations ranged from 5800 to 37 000 genome copies m . On average, 64 per cent of the viral genome copies were associated with fine particles smaller than 2.5 μm, which can remain suspended for hours. Modeling of virus concentrations indoors suggested a source strength of 1.6 ± 1.2 × 105 genome copies m−3 air h−1 and a deposition flux onto surfaces of 13 ± 7 genome copies m−2 h−1 by Brownian motion. Over one hour, the inhalation dose was estimated to be 30 ± 18 median tissue culture infectious dose (TCID50), adequate to induce infection. These results provide quantitative support for the idea that the aerosol route could be an important mode of influenza transmission.”
Such small particles (< 2.5 μm) are part of air fluidity, are not subject to gravitational sedimentation, and would not be stopped by long-range inertial impact. This means that the slightest (even momentary) facial misfit of a mask or respirator renders the design filtration norm of the mask or respirator entirely irrelevant. In any case, the filtration material itself of N95 (average pore size ~0.3−0.5 μm) does not block virion penetration, not to mention surgical masks. For example, see Balazy et al. (2006).
Mask stoppage efficiency and host inhalation are only half of the equation, however, because the minimal infective dose (MID) must also be considered. For example, if a large number of pathogen-laden particles must be delivered to the lung within a certain time for the illness to take hold, then partial blocking by any mask or cloth can be enough to make a significant difference.
On the other hand, if the MID is amply surpassed by the virions carried in a single aerosol particle able to evade mask-capture, then the mask is of no practical utility, which is the case.
Yezli and Otter (2011), in their review of the MID, point out relevant features:
All of this to say that: if anything gets through (and it always does, irrespective of the mask), then you are going to be infected. Masks cannot possibly work. It is not surprising, therefore, that no bias-free study has ever found a benefit from wearing a mask or respirator in this application.
- Most respiratory viruses are as infective in humans as in tissue culture having optimal laboratory susceptibility
- It is believed that a single virion can be enough to induce illness in the host
- The 50-percent probability MID (“TCID50”) has variably been found to be in the range 100−1000 virions
- There are typically 10 to 3rd power − 10 to 7th power virions per aerolized influenza droplet with diameter 1 μm − 10 μm
- The 50-percent probability MID easily fits into a single (one) aerolized droplet
- For further background:
- A classic description of dose-response assessment is provided by Haas (1993).
- Zwart et al. (2009) provided the first laboratory proof, in a virus-insect system, that the action of a single virion can be sufficient to cause disease.
- Baccam et al. (2006) calculated from empirical data that, with influenza A in humans,“we estimate that after a delay of ~6 h, infected cells begin producing influenza virus and continue to do so for ~5 h. The average lifetime of infected cells is ~11 h, and the half-life of free infectious virus is ~3 h. We calculated the [in-body] basic reproductive number, R0, which indicated that a single infected cell could produce ~22 new productive infections.”
- Brooke et al. (2013) showed that, contrary to prior modeling assumptions, although not all influenza-A-infected cells in the human body produce infectious progeny (virions), nonetheless, 90 percent of infected cell are significantly impacted, rather than simply surviving unharmed.
Therefore, the studies that show partial stopping power of masks, or that show that masks can capture many large droplets produced by a sneezing or coughing mask-wearer, in light of the above-described features of the problem, are irrelevant. For example, such studies as these: Leung (2020), Davies (2013), Lai (2012), and Sande (2008).
Why There Can Never Be an Empirical Test of a Nation-Wide Mask-Wearing Policy
As mentioned above, no study exists that shows a benefit from a broad policy to wear masks in public. There is good reason for this. It would be impossible to obtain unambiguous and bias-free results [because]:
Unknown Aspects of Mask Wearing
- Any benefit from mask-wearing would have to be a small effect, since undetected in controlled experiments, which would be swamped by the larger effects, notably the large effect from changing atmospheric humidity.
- Mask compliance and mask adjustment habits would be unknown.
- Mask-wearing is associated (correlated) with several other health behaviors; see Wada (2012).
- The results would not be transferable, because of differing cultural habits.
- Compliance is achieved by fear, and individuals can habituate to fear-based propaganda, and can have disparate basic responses.
- Monitoring and compliance measurement are near-impossible, and subject to large errors.
- Self-reporting (such as in surveys) is notoriously biased, because individuals have the self-interested belief that their efforts are useful.
- Progression of the epidemic is not verified with reliable tests on large population samples, and generally relies on non-representative hospital visits or admissions.
- Several different pathogens (viruses and strains of viruses) causing respiratory illness generally act together, in the same population and/or in individuals, and are not resolved, while having different epidemiological characteristics.
Many potential harms may arise from broad public policies to wear masks, and the following unanswered questions arise:
Conclusion
- Do used and loaded masks become sources of enhanced transmission, for the wearer and others?
- Do masks become collectors and retainers of pathogens that the mask wearer would otherwise avoid when breathing without a mask?
- Are large droplets captured by a mask atomized or aerolized into breathable components? Can virions escape an evaporating droplet stuck to a mask fiber?
- What are the dangers of bacterial growth on a used and loaded mask?
- How do pathogen-laden droplets interact with environmental dust and aerosols captured on the mask?
- What are long-term health effects on HCW, such as headaches, arising from impeded breathing?
- Are there negative social consequences to a masked society?
- Are there negative psychological consequences to wearing a mask, as a fear-based behavioral modification?
- What are the environmental consequences of mask manufacturing and disposal?
- Do the masks shed fibers or substances that are harmful when inhaled?
By making mask-wearing recommendations and policies for the general public, or by expressly condoning the practice, governments have both ignored the scientific evidence and done the opposite of following the precautionary principle.
In an absence of knowledge, governments should not make policies that have a hypothetical potential to cause harm. The government has an onus barrier before it instigates a broad social-engineering intervention, or allows corporations to exploit fear-based sentiments.
Furthermore, individuals should know that there is no known benefit arising from wearing a mask in a viral respiratory illness epidemic, and that scientific studies have shown that any benefit must be residually small, compared to other and determinative factors.
Otherwise, what is the point of publicly funded science?
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
Denis G. Rancourt is a researcher at the Ontario Civil Liberties Association (OCLA.ca) and is formerly a tenured professor at the University of Ottawa, Canada. This paper was originally published at Rancourt's account on ResearchGate.net. As of June 5, 2020, this paper was removed from his profile by its administrators at Researchgate.net/profile/D_Rancourt. At Rancourt's blog ActivistTeacher.blogspot.com, he recounts the notification and responses he received from ResearchGate.net and states, “This is censorship of my scientific work like I have never experienced before.”
The original April 2020 white paper in .pdf format is available here, complete with charts that have not been reprinted in the Reader print or web versions.
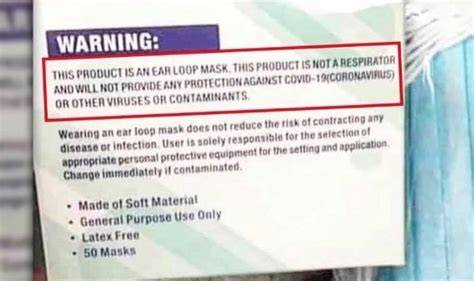
View attachment 1715654897
Real science beats the lying nanny state control freaks every time.
norshorblufish
By the Big Water
No one said these masks are the cure all to stop it.
They help control the aerosol spray produced by talking, sneezing, and coughing. It means if you wear one you have somewhat of a chance of not spreading or getting it then not wearing one.
As far as the curve goes. Yes it lengths the time period, it doesn't mean less people will get it. It means that it gives the medical facilities a better chance to to treat more people over that period and not put a strain on them. Which mean possibly more people would survive it.
If people would also understand that not going to crowded areas such as parties, bars,rallies, etc. would help too. Which is just plain common sense
which appears that a lot of people in this world don't use.
They help control the aerosol spray produced by talking, sneezing, and coughing. It means if you wear one you have somewhat of a chance of not spreading or getting it then not wearing one.
As far as the curve goes. Yes it lengths the time period, it doesn't mean less people will get it. It means that it gives the medical facilities a better chance to to treat more people over that period and not put a strain on them. Which mean possibly more people would survive it.
If people would also understand that not going to crowded areas such as parties, bars,rallies, etc. would help too. Which is just plain common sense
which appears that a lot of people in this world don't use.
ir3333
Well-Known Member
i agree.If you cough or breath with a mask on it will not stop air travel but will reduce the distance it travels and those properly distancing are less likely to be infected.I can't believe the extremes some are going to, to berate something so simple and easy to do. Is there any value in wearing a mask to make family, friends and people around you more comfortable?
Divenut
Well-Known Member
Wonder why most people cover there mouth when they cough? Though from some of the replies, it would seem some folks probably don't do that either. Kinda like the morons that openly hack and cough all over everyone on public transportation. Anti-maskers should have no problem with others spewing their cold and flu bug infested spittle on them while riding the train, bus etc correct? I mean, you clearly can not have a problem with that based on your attempts to illegitimize any positive affects of masking up during the pandemic.
yellow rose
Overnight Sensation
Wonder why most people cover there mouth when they cough? Though from some of the replies, it would seem some folks probably don't do that either. Kinda like the morons that openly hack and cough all over everyone on public transportation. Anti-maskers should have no problem with others spewing their cold and flu bug infested spittle on them while riding the train, bus etc correct? I mean, you clearly can not have a problem with that based on your attempts to illegitimize any positive affects of masking up during the pandemic.
I you don’t understand the control you are under for nothing more than a flu then you deserve to wear a mask that does nothing.
Cuda416
Well-Known Member
An observation....
I keep seeing proponents of mask mandates claiming those of us against the MANDATES, give people wearing masks a hard time....
Not even close... We as a group disagree with you, but we don't run around giving people crap because they choose to wear one. Now, I might complain and call you mask folks silly in forums, but I'll point back to my own posts, you can find them, in which I say if you want to wear one, knock yourself out.
The reverse however is NOT true. I've been called names in public places to my face and generally been given crap for not wearing one by people who want to force me to wear one.... How many times in this and the other thread have we been called "anti maskers" and generally characterized as heartless or selfish? Lots, go look...
Now, once again.... I'll type SLOW.... If you want to wear a mask, go for it. Don't force me to..... after all, no one is trying to FORCE you to NOT wear one.
I keep seeing proponents of mask mandates claiming those of us against the MANDATES, give people wearing masks a hard time....
Not even close... We as a group disagree with you, but we don't run around giving people crap because they choose to wear one. Now, I might complain and call you mask folks silly in forums, but I'll point back to my own posts, you can find them, in which I say if you want to wear one, knock yourself out.
The reverse however is NOT true. I've been called names in public places to my face and generally been given crap for not wearing one by people who want to force me to wear one.... How many times in this and the other thread have we been called "anti maskers" and generally characterized as heartless or selfish? Lots, go look...
Now, once again.... I'll type SLOW.... If you want to wear a mask, go for it. Don't force me to..... after all, no one is trying to FORCE you to NOT wear one.
Divenut
Well-Known Member
Yeah, I could care less if anyone wears a mask or not. Folks are wired differently, I get it.. Though I do appreciate and respect the folks that have the decency to wear them in public when in close proximity to me and my family. A civil courtesy if you will.
Cuda416
Well-Known Member
Yeah, I could care less if anyone wears a mask or not. Though do appreciate and respect the folks that have the decency to wear them in public when in close proximity to me and my family. A civil courtesy if you will.
Fair enough, and I appreciate the folks who have the decency to keep their trap shut and not call my wife, who has an actual reason for not wearing one, a selfish asshole... then scurrying away like a cockroach...
yellow rose
Overnight Sensation
Yeah, I could care less if anyone wears a mask or not. Folks are wired differently, I get it.. Though I do appreciate and respect the folks that have the decency to wear them in public when in close proximity to me and my family. A civil courtesy if you will.
I get that. But if the mask works, your mask will save you. That’s my point. The pro maskers think you are smart enough to make decisions for me that have no affect on you. I’ve neber had the desire to impose my will on someone else. Especially when it steps on a freedom. Your freedom stops where my freedom begins and that means I don’t have to live in abject fear imposed by a tyrannical, despotic government.
It’s too bad the pro maskers don’t extend the same courtesy.
Divenut
Well-Known Member
Agreed Cuda416. Much of the country seems to have recently been embolden to say and do things they might not have in the past. It's like society has lost the ability to discuss things in a rational, civil manner. Hopefully, we as a country can find a way to recapture some of that solidarity and comradery we lost.
Cuda416
Well-Known Member
Agreed Cuda416. Much of the country seems to have recently been embolden to say and do things they might not have in the past. It's like society has lost the ability to discuss things in a rational, civil manner. Hopefully, we as a country can find a way to recapture some of that solidarity and comradery we lost.
Agreed, I believe it started with social media as we know it and the hog pile approach people tend to take these days. The more "likes" etc people get, it seems to re-enforce their perception on how correct they are. Doesn't really wash when they are surrounded by people who already agree with them. It just serves to stroke egos. Right or Wrong, doesn't matter to those people in those circumstances, only what they see as popular opinion.
ir3333
Well-Known Member
I you don’t understand the control you are under for nothing more than a flu then you deserve to wear a mask that does nothing.
Control...there is no control. No matter what law is passed you and i both decide whether or not to abide by it.
No one ever does anything they don't want to.
-